Keeping the Cornea in Shape
UT Health Austin ophthalmologists share the importance of taking a proactive approach to keratoconus treatment
Reviewed by: Eileen Bowden, MD, and Gene Kim, MD
sWritten by: Lauren Schneider
Does your vision seem blurrier than usual? While common ophthalmologic conditions, such as cataracts or glaucoma, may be the culprit, patients and providers should not rule out keratoconus, which is caused by thinning of the cornea, the protective outer layer of the eye that regulates how light passes into the eye.
According to the American Academy of Ophthalmology, keratoconus reportedly affects 1 in 700 people. However, the real prevalence of the condition is thought to be much higher.
“In my experience, keratoconus is more common than many people realize,” shares Gene Kim, MD, a board-certified ophthalmologist in UT Health Austin’s Mitchel and Shannon Wong Eye Institute. Dr. Kim specializes in corneal transplants and surgical reconstruction of the anterior segment, the frontmost portion of the eye comprised of the cornea, iris, and lens.
“Recognizing and addressing keratoconus in a timely manner can help patients prevent further visual impairment,” adds Dr. Kim.
Hear from UT Health Austin ophthalmologists as they answer questions from social media about eye health.
<br>Gradual Damage to the Cornea
Keratoconus is closely related to astigmatism, a more well-known condition involving irregularities in the shape of the cornea or lens. “Many of the patients I treat for astigmatism experience some degree of keratoconus,” observes Dr. Kim. “Patients with keratoconus have astigmatism, but not everyone with astigmatism has keratoconus.”
“Keratoconus describes a specific pattern of corneal dysfunction: a thinning of the tissue that causes the cornea to bulge from its typical sphere shape to more of a basketball shape,” explains Eileen Bowden, MD, a board-certified ophthalmologist in the Mitchel and Shannon Wong Eye Institute, who specializes in glaucoma and anterior segment conditions, including cataracts. “Over time, this distortion results in blurry vision.”
Symptoms of keratoconus may include:
- Blurred or reduced vision
- Difficulty seeing at night
- Eye pain, possibly with associated headaches
- Halos around bright lights and/or increased sensitivity to bright light
While keratoconus can affect patients of all ages and backgrounds, some people are at greater risk for the condition than others. “People with certain genetic syndromes, such as Down’s syndrome, are more likely to develop keratoconus,” notes Dr. Bowden.
Another major risk factor for the condition is allergies, which are associated with excessive eye rubbing that may wear down the cornea over time. “If you have severe allergies, you can reduce your risk of keratoconus if you avoid rubbing your eyes,” says Dr. Bowden.
Stay ahead of allergy symptoms year-round with these tips.
<br>Regardless of cause, keratoconus typically develops when a patient is an adolescent or young adult. Symptoms may grow more pronounced as the condition progresses and the structural integrity of the cornea becomes even more compromised.
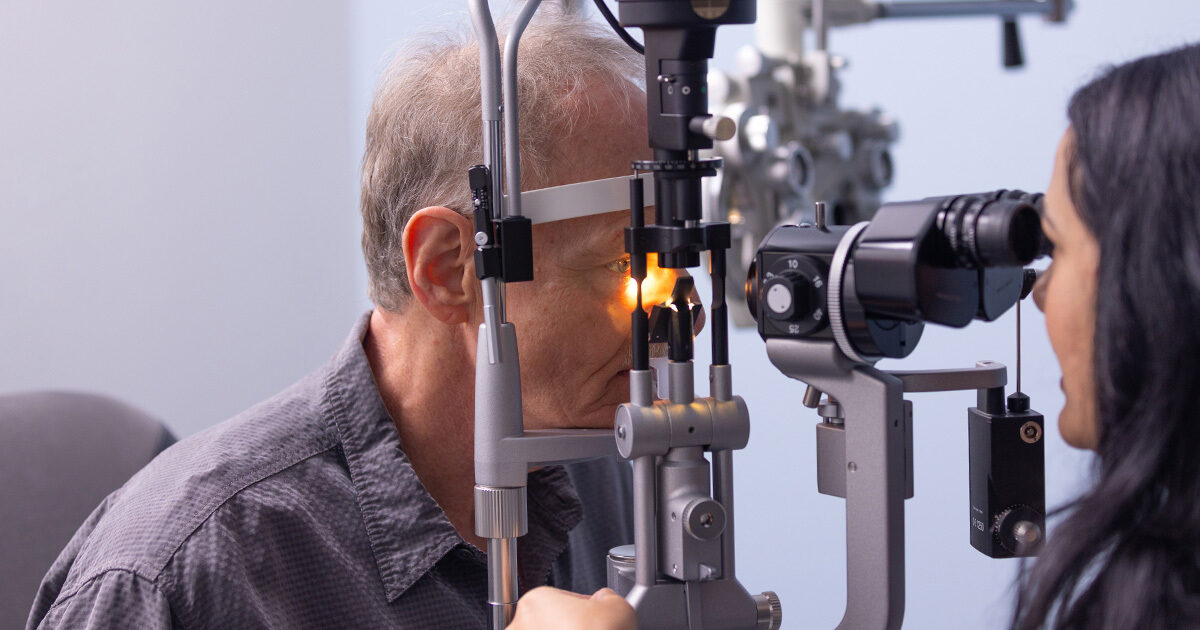
“Keratoconus is typically diagnosed with the aid of a microscope during an eye exam, but in severe cases, the cornea is so misshapen that the condition can be detected with the naked eye,” shares Dr. Bowden.
Personalized, Proactive Keratoconus Management
Because keratoconus symptoms worsen over time, early diagnosis and treatment are key for the best outcomes. “If you start to notice changes to your vision, you should schedule an eye exam right away,” recommends Dr. Bowden. “An ophthalmologist can diagnose and treat keratoconus or other conditions that may be affecting your eyesight.”
Explore the benefits of annual eye exams.
<br>Dr. Kim treats advanced cases of keratoconus requiring corneal transplant surgery in which a patient’s weakened cornea is replaced with healthy donor tissue. “Healthy corneal tissue focuses light properly as it enters the eye, helping restore a patient’s vision,” says Dr. Kim.
“A patient’s experience during treatment and recovery may vary depending on how much of the corneal tissue is replaced,” adds Dr. Kim. “However, most corneal transplants are completed in under an hour and patients often return home the same day.”
Patients receiving corneal transplant at the Mitchel and Shannon Wong Eye Institute may undergo treatment at the Ambulatory Surgery Center (ASC), UT Health Austin’s state-of-the-art facility for outpatient and select short-stay surgical procedures. “In addition to the great support the ASC care team offers surgeons, the center allows our patients to undergo corneal transplant in the same convenient location where they receive the rest of their ophthalmologic care,” notes Dr. Kim.
The Mitchel and Shannon Wong Eye Institute care team can also refer patients to providers who treat less advanced forms of keratoconus. Many of these cases are treated using specialty contact lenses that hold the cornea in a more rounded shape. Other patients may opt for a procedure called corneal cross-linking in which a laser is used to strengthen the corneal tissue.
“Corneal cross-linking cannot restore a patient’s vision, but it can help prevent their condition from progressing,” explains Dr. Bowden. “This procedure is especially beneficial to young patients, whose keratoconus would otherwise worsen over their lifespan. It also offers a useful alternative for patients who cannot tolerate contact lenses.”
Dr. Bowden answers common questions about glaucoma prevention, diagnosis, and treatment.
<br>Whether keratoconus is corrected surgically at UT Health Austin or through another approach at a different practice, the Mitchel and Shannon Wong Eye Institute care team helps patients access the treatment option best suited to their unique needs.
“Our providers work with patients experiencing keratoconus and other ophthalmologic conditions to determine the best course of action,” says Dr. Kim. “We believe the highest standard of eye care comes through an individualized approach that accounts for a patient’s symptoms, health background, and personal preferences.”
For more information about the Mitchel and Shannon Wong Eye Institute or to request an appointment, call 1-833-UT-CARES (1-833-882-2737) or visit here.