Taking a Comprehensive Approach to Patient Care
UT Health Austin’s Musculoskeletal Institute delivers whole-person care to patients across the Central Texas community
Reviewed by: J. Mica Guzman, Jr., MD, MBA, DABFM, CAQSM
Written by: Erich Pelletier and Abbi Havens
At UT Health Austin’s award-winning Musculoskeletal Institute, continuity of care is a leading concern and goal. Continuity of care is the patient-centered method through which a patient’s care team is involved in determining the most effective and sustainable path for the patient’s care over time. This method leverages the expertise and experience of all the providers on the team to ensure the patient receives not only the most comprehensive guidance and care of the highest quality, but also an experience that is often more convenient and the most cost-effective.
J. Mica Guzman, MD, MS, DABFM, RMSK, CAQSM, a board-certified sports medicine specialist and the Primary Care Sports Medicine Clinical Director for the Sports and Injury Clinic within UT Health Austin’s Musculoskeletal Institute, places continuity of care at the top of his list of priorities. He also serves as the Clinical Director for both Bone Health and Concussion Care within the Musculoskeletal Institute and the Medical Director of Sports Medicine and Events Coverage for the Musculoskeletal Institute.“ Just yesterday, we had a patient who was referred to us for an imaging review of her femur, the large bone in the thigh, along with concerns of a quadriceps strain,” shares Dr. Guzman. ”She also met with me for care of persistent post-concussion symptoms. After we reviewed her imaging, she was able to visit with our physical therapist about her quadriceps strain. She received direct coordination of care to her primary doctor and her specialists. And this all took place within the one appointment.”
“The benefit of this multidisciplinary care model,” explains Dr. Guzman, “is that we don’t just see the patients who come into the clinic for their presenting complaint. We collaborate and coordinate patient care with their primary care or referring physician and involve other specialists through patient referrals if the issue is beyond our expertise or focus.”
At UT Health Austin, patients benefit from the expertise of multiple specialists across a variety of disciplines caring for them in one place. Where possible, we have redesigned the care model to enable patients to see multiple specialists during the same visit depending on their specific health needs. This makes it easier for you to get the care you need without having to make multiple trips to various locations.

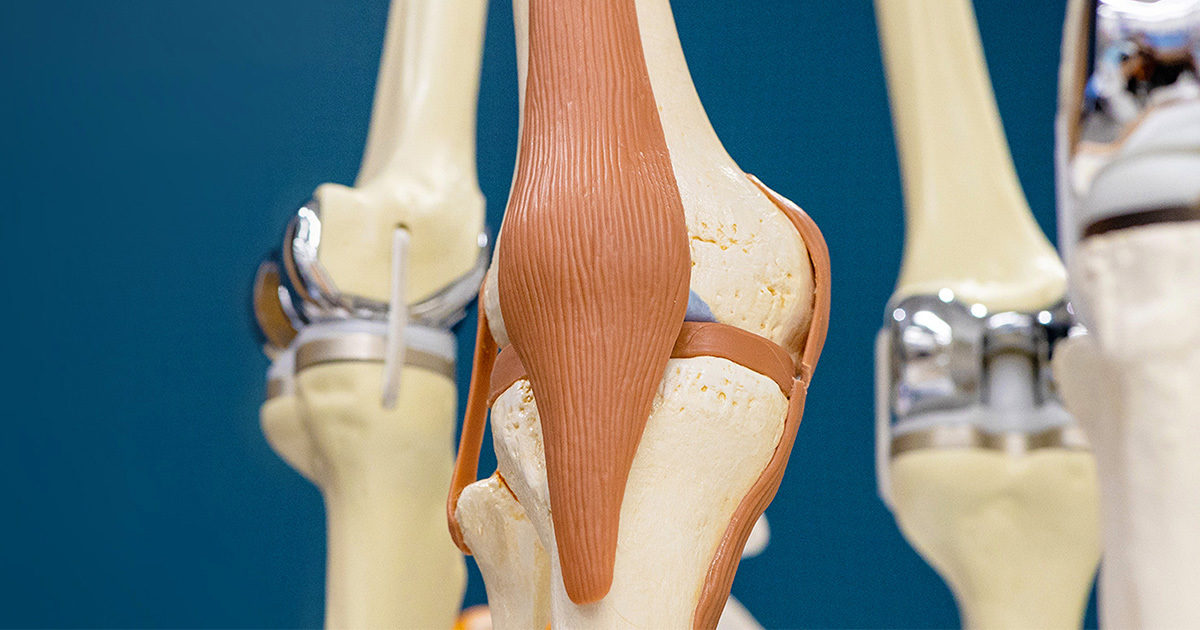
The Musculoskeletal Institute care team includes orthopedic surgeons, sports medicine physicians, physician assistants, physical therapists, physiatrists (physical medicine and rehabilitation specialists), chiropractors, nurse practitioners, dietitians, social workers, and more.
Providers at the Musculoskeletal Institute also collaborate with colleagues at the Dell Medical School and The University of Texas at Austin to apply the latest research, diagnostic, and treatment techniques, allowing them to customize a treatment plan specific to each patient. Treatment may include nonsurgical interventions, such as lifestyle modifications, physical therapy, or medication and injections, or surgery. Advanced imaging and lab testing are also available on-site.
Continuity Through Technology
This comprehensive approach to health care manifests not only through the physicians and staff working at the Musculoskeletal Institute, but also through the technologies available in the clinic. Among the state-of-the-art tools used by the Musculoskeletal Institute is the GE Lunar DXA, a low-dose X-ray scanner. The DXA scanner provides crisp, high resolution images of a patient’s hip, femur, and lower spine (as well as the forearm if a patient’s prosthetic implants preclude a clean hip scan) that are used to determine bone density. The scans are quick, painless, and safe.
“The scanner looks at the bone contour and essentially subtracts the soft tissue from that image,” explains Dr. Guzman. “Then, it produces a score report, which is really like a standard deviation compared to an ideal bone density.”
Put simply, the DXA scanner measures the amount of “good bone” a patient has left and provides the radiologist with a bone density score, adjusted for sex and age. Patients who are below a certain bone density score may be at a higher risk for bone fractures. With its high-resolution capabilities, the machine is also able to detect small but significant changes sooner, allowing for preventative and proactive care.
Adults over the age of 65 (particularly women) or any person who has reason to be concerned about osteoporosis, including those suffering from certain cancers or diseases or medications that result in bone loss, should consider a bone density screening. Because the machine provides a more automated process than ever before, patients often receive better results at a fraction of the cost.
Primary Interventions, Preventative Care
Beyond expertise and equipment, the notion of continuity also extends “backwards” in time to include preventative care and patient behavior. “Building maximum bone mass happens decades before you ever receive an osteoporosis diagnosis,” says Dr. Guzman. “It really happens when we’re growing up, in our childhood.”
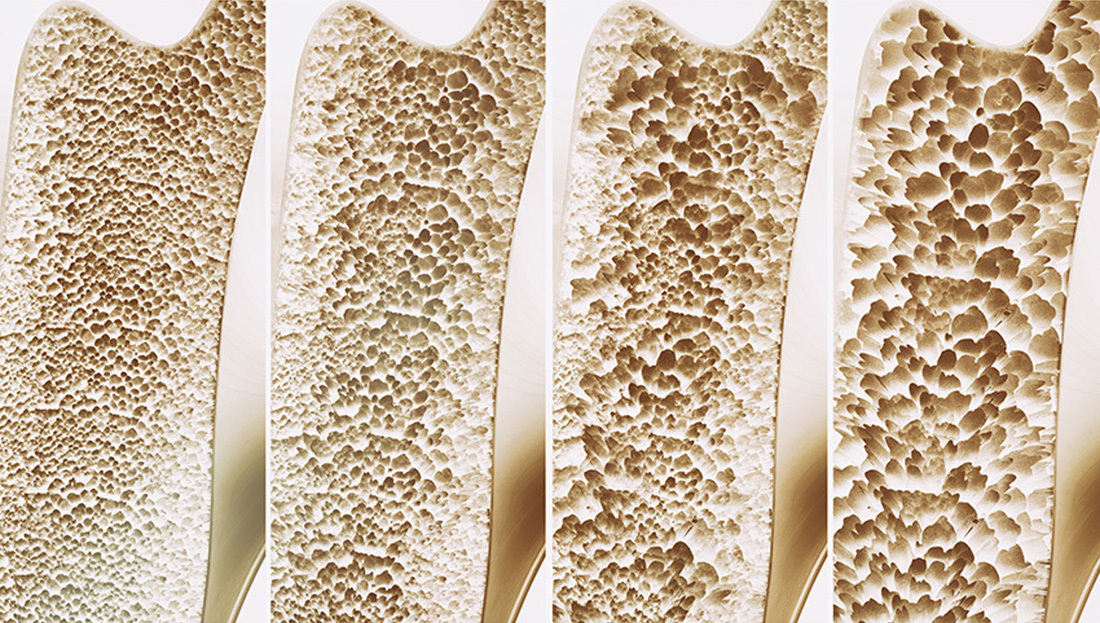
Osteoporosis is a disease in which bone mass is reduced and bones become more porous than is typical, leaving bones weak and prone to fracture. While some decrease in bone mass is an expected part of the natural aging process, osteoporosis can lead to stooped posture, pain, and acute mobility challenges.
To combat osteoporosis, Dr. Guzman recommends a mix of appropriate diet, supplements if necessary, and exercise. “Primary prevention would be optimizing that calcium intake, optimizing that Vitamin D intake, optimizing exercise and impact activities in those years, decades really, preceding a diagnosis,” says Dr. Guzman. “Too many times, we see that optimization or impact activities didn’t happen, and now we’re seeing the results in our aging population.”
Exercise and “impact activities” are critical to bone health, and they do not have to be heavy exercise to be effective. “Bone is constantly remodeling itself,” explains Dr. Guzman, “and it needs to know where to delegate resources. That delegation happens with stress on the bone.”
“It doesn’t necessarily mean you have to go to the gym and lift weights,” continues Dr. Guzman. “Walking is an impact activity because your feet are impacting the ground. A lot of people ask whether running is more impactful, and yes, it is, but any impact activity is a benefit, as it increases the stress or load of muscle tissue pulling on the bone.”
Learn more about maintaining bone health.
<br>Community Care
The idea of continuity of care also extends beyond the clinical practice and into the Central Texas community.
Dr. Guzman and other members of the Musculoskeletal Institute care team often provide sideline medical coverage to local sports teams, including coverage for football and other contact sports at Austin High School and for athletics at The University of Texas at Austin.
“We take residents and medical students who are interested in sports medicine with us to these events,” shares Dr. Guzman. ”I also help out with mass event coverage, the most recent one being the 3M Half Marathon here in Austin and the Iron Man Triathlon in Waco. I’ve been thankful to be a part of that and witness these athletes compete for glory.”
Through multidisciplinary expertise, state-of-the-art technology, behavioral guidance, and community support and engagement, UT Health Austin’s Musculoskeletal Institute provides “whole-person” continuity of care to patients across Central Texas.
To learn more about the Musculoskeletal Institute or make an appointment, call 1-833-UT-CARES (1-833-882-2737) or visit here.