About Osteoporosis
In addition to its mechanical function, bone serves as a reservoir, or storage space, for calcium, phosphorus, and other minerals. Calcium and phosphorous work in conjunction with vitamin D to build and break down skeletal tissue to keep bones healthy and strong. New bone tissue is created to balance the amount of bone tissue broken down and absorbed by the body in a natural process known as bone turnover, or bone remodeling. Throughout the early part of our lives, the amount of bone loss and the amount of bone gained remain balanced. Once individuals reach peak bone mass (size and thickness), more bone is broken down than is formed, causing the bone mass to slowly start to decline.
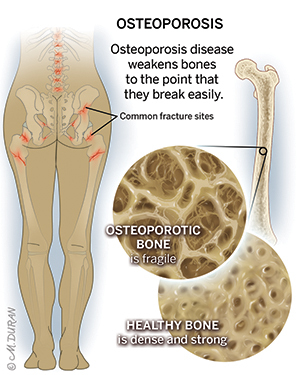
The amount of calcium and other minerals present in your bones is called bone density. The higher your bone density, the stronger your bones will become. Your body is best at storing calcium in your bones while you are young, so most people reach peak bone density between the ages of 25 and 30. The higher your peak bone mass, the less likely you are to develop osteoporosis, a state of low bone density that causes the bone to be weak and brittle and makes fracturing (breaking) your bones much more likely, which can put you at an increased risk for fragility fractures. Fragility fractures are broken bones that occur when a low impact or minimal stress is placed on the bone, such as from a fall from standing height or less or even a cough or sneeze, that would not normally result in a fracture.
After peak bone density is achieved, the bone remodeling process continues, but bones will naturally lose density over time. Your likelihood of developing osteoporosis depends on the amount of minerals stored in your bones from peak bone density and how your body uses those minerals in the years that follow.
Symptoms of Osteoporosis
Many people with osteoporosis have no obvious symptoms and do not realize they have the condition until they fracture a bone. For this reason, people at risk for osteoporosis should have their bone density measured regularly.
Symptoms of osteoporosis may include:
- Fragility fractures (broken bones that occur when a low impact or minimal stress is placed on the bone– such as from a fall from standing height or less or even a cough or sneeze– that would not normally result in a fracture).
Risk Factors for Osteoporosis
While osteoporosis affects people of all ages, sexes, and backgrounds, certain people are more likely to develop the condition.
Risk factors for osteoporosis may include:
- Age: Older adults are more susceptible to osteoporosis. Women over the age of 65 and men over the age of 70 are at the highest risk.
- Family history: Genetics can contribute to the risk for osteoporosis. A family history in a person’s mother or father can increase the risk for osteoporosis and osteoporotic fractures as well as negatively affect bone mineral density.
- Health history: People with a history of hormonal or gastrointestinal conditions, eating disorders, rheumatoid arthritis, HIV/AIDS, and certain types of cancer are more likely to develop osteoporosis, as are people who use medications such as thiazolidinediones, selective serotonin reuptake inhibitors (SSRIs), antiepileptic medications, glucocorticoids, adrenotropic hormones, and certain cancer medications.
- Personal history: Osteoporosis is linked to low dietary intake of calcium and vitamin D, a lack of regular exercise, smoking, and heavy alcohol consumption.
- Sex: Osteoporosis is more common in female patients. Not only do women tend to have a lower peak bone mass, but the decrease in estrogen during menopause can also affect bone density.
Diagnosing Osteoporosis
Osteoporosis can be diagnosed with a dual-energy X-ray absorptiometry (DEXA) scan, also referred to as a bone mineral density scan, which is a form of X-ray imaging that measures bone mineral density. Individuals at risk for osteoporosis are recommended to undergo a DEXA scan every 2-5 years.
Treating Osteoporosis at UT Health Austin
Your bone health is dependent on multiple factors. If you have concerns related to your bone health due to a diagnosis of osteoporosis or you have suffered a fragility fracture, preventative measures can help avoid future injury. Treatment may involve a combination of a cast or brace, surgery, rehabilitation, exercise and diet recommendations, prescribed medications, supplement guidance, and more. Your doctor will work with you to determine the best course of action.
Care Team Approach
At UT Health Austin, we take a multidisciplinary approach to your care. This means you will benefit from the expertise of multiple specialists across a variety of disciplines caring for you in one place to avoid having to schedule multiple appointments with providers at locations all over the city. The Musculoskeletal Institute care team includes orthopedic surgeons, sports medicine physicians, physician assistants, physical therapists, physiatrists, chiropractors, nurse practitioners, dietitians, social workers, and more who work together to help you get back to the things in your life that matter most to you.
We collaborate with our colleagues at the Dell Medical School and The University of Texas at Austin to utilize the latest research, diagnostic, and treatment techniques, allowing us to customize a treatment plan specific to you. Advanced imaging and lab testing are also available on-site if needed.
Learn More About Your Care Team

Musculoskeletal Institute
Health Transformation Building, 9th Floor
1601 Trinity Street, Bldg. A, Austin, Texas 78712
1-833-UT-CARES (1-833-882-2737)
Get Directions