The Power of Personalized Care
UT Health Austin neurologist improves MS diagnosis and care through patient-provider relationships
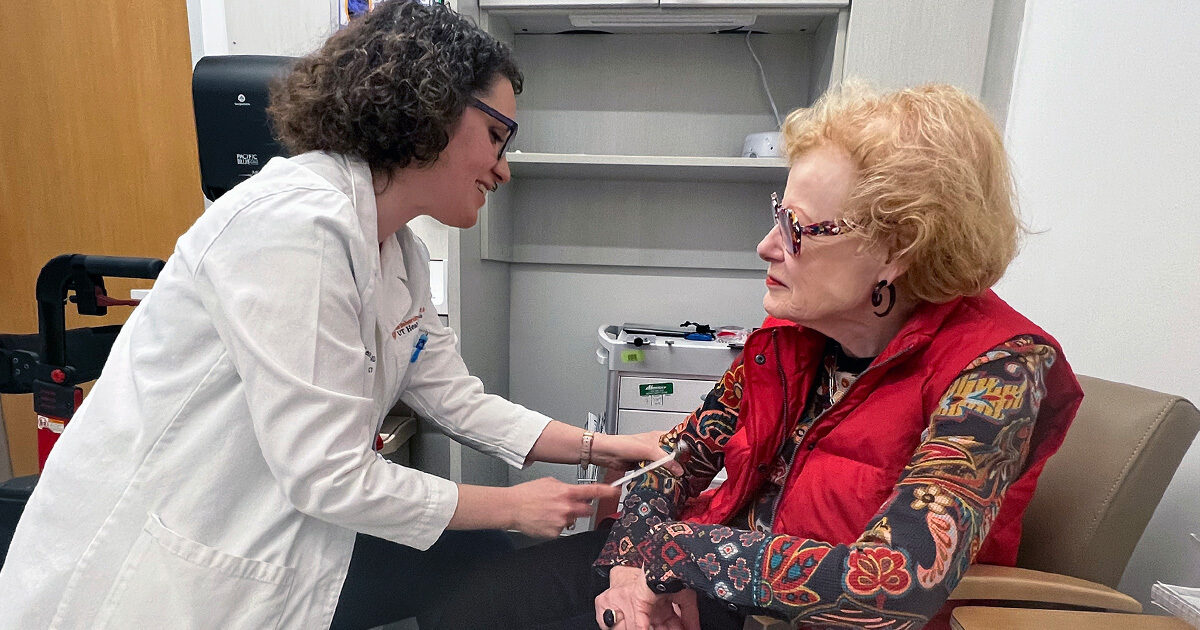
Reviewed by: Vicki Aymond and Léorah Freeman MD, PhD
Written by: Ashley Lawrence
In August of 2010, Vicki Aymond was diagnosed with primary progressive multiple sclerosis (PPMS). “I was 58 at the time of my diagnosis,” shares Vicki. “Most people are diagnosed by the age of 40, which is why it’s considered a ‘young person’s’ disease. Chances are I had been living with MS for many years but never picked up on the hidden signs.”
MS is a chronic neurological disease that impacts the central nervous system, which is composed of the brain and spinal cord. In MS, the body’s immune system has an abnormal response to the central nervous system. This causes inflammation and damage to myelin, a fatty material that protects your nerves, which can result in communication problems between the brain and the rest of the body. While a range of available treatments may decrease the risk of MS worsening over time and can help MS patients manage their symptoms, there is currently no cure for the disease.
Learn more about multiple sclerosis.
<br>Diagnosing MS in Older Adults
“MS is one of the more challenging illnesses to diagnose, because it can look very different from person to person,” explains Vicki. People diagnosed with MS often experience a wide range of debilitating symptoms, including loss of motor function, cognitive dysfunction, ongoing tissue inflammation and pain, and more, depending on the amount of nerve damage that exists and which nerves are affected.
Diagnosing MS in older adults can be particularly challenging because some symptoms of MS mirror the normal signs of aging, such as muscle weakness, balance problems, fatigue, vision changes, hearing loss, and difficulty sleeping. “I find that a lot of doctors will try to attribute my symptoms to my age,” says Vicki. “They’ll tell me, ‘You know, you are 70 now.’ Well, I know how old I am. I also know myself and my body. Not everything is a result of getting older.”
MS changes with age, increasing the complexity of care for older patients, who are not only at higher risk of progression of the disease, but also more susceptible to complications from immunosuppressive therapies. Despite these unique challenges faced by older patients, relatively little research focuses on people with MS who are over the age of 50. Léorah Freeman MD, PhD, a neurologist in UT Health Austin’s Multiple Sclerosis and Neuroimmunology Center within the Mulva Clinic for the Neurosciences, is working to change that.
Learn more about Dr. Freeman’s research that focuses on patients with MS who are over the age of 50.
<br>Establishing Patient-Provider Relationships
“My husband likes to tease me by saying, ‘Every time you walk into a doctor’s office you want to chit-chat.’” shares Vicki. “It’s important to me that my doctors know who I am. I want them to know that I have two grandchildren and another grandchild on the way. I want them to know that while I may not be able to pick up and carry this new baby, there are others way for me to be involved, and I intend to pursue and explore these opportunities. These are little things that I’m suddenly thinking about that I would never have thought about before and that other people often don’t think about either.”
At UT Health Austin, we put you, your family, and your needs at the forefront of your care. Our experienced healthcare professionals deliver personalized, whole-person care of uncompromising quality and treat each patient as an individual with unique circumstances, priorities, and beliefs. Working with you, your care team creates an individualized care plan to help you reach the goals that matter most to you — in the care room and beyond.
“The first time I met with Dr. Freeman, I asked myself, ‘Did I get the luck of the draw?’” says Vicki. “Because she gave up three hours of her time to listen and truly hear what I had to say. She sat with me, took handwritten notes, and repeated things back to me to make sure she had an accurate record of what I was telling her. I kept thinking, ‘Surely another patient is waiting out in the hall.’ Of course, that wasn’t the case, but I had become accustomed to doctors spending 15 minutes with me before checking me off their list.”
Dr. Freeman works alongside several clinicians, including other neurologists, advanced practice providers, health social workers, registered dietitians, nurses, and more. “By bringing a team together to meet the needs of our patients, we’re not only listening one-on-one, but we’re also listening collectively,” explains Dr. Freeman. “This can make a huge difference in the coordination of care.”
Understanding the Value of Academic Medicine
In the last 12 years, in addition to her MS diagnosis, Vicki has developed chronic pain in the left top quadrant of her back that has since spread to her left shoulder and down to her left elbow. During the COVID-19 pandemic, she was also diagnosed with breast cancer and is currently in remission. However, despite years of appointments with various specialists and experimenting with countless treatment options, the chronic pain on the left side of Vicki’s body persists, and she has yet to receive any confirmation as to whether the pain is related to her MS diagnosis or something else entirely.
“What I love about Dr. Freeman most is that she’s a physician-researcher,” shares Vicki. “She’s immersed in research daily, and the chronic pain that I’m still experiencing today is something that needs to be regularly studied and researched or it’ll continue to go undetected. And when I asked Dr. Freeman if there would be a problem with me reaching out to other doctors and research centers for answers to what is causing my pain, she immediately said, ‘Absolutely not. The more people that we can get to listen, the closer we can get to finding answers.’ Dr. Freeman truly is the best of the best.”
Dr. Freeman is an assistant professor in the Dell Medical School Department of Neurology and a courtesy assistant professor in the Dell Medical School Department of Diagnostic Medicine. She also serves as the Director of the Multiple Sclerosis Imaging and Outcomes Research Laboratory at the Dell Medical School.
“MS isn’t a disease that can easily be resolved or fixed,” warns Vicki. “Currently, there is no ‘fixing.’ There are modifying drugs that help to delay or manage the disease, but no cure for MS, which is why it’s important that you advocate for yourself. My advice to others would be to speak up and be willing to go the whole nine yards. You know your body better than anyone, and when it’s telling you something, listen! Don’t be afraid to seek out a second and third opinion until you find a provider that values what you have to say. You have to advocate for your voice to be heard. Patients have to listen to their doctors and doctors have to listen to their patients.”
For more information about the Multiple Sclerosis and Neuroimmunology Center or to schedule an appointment, call 1-833-UT-CARES (1-833-882-2737) or visit here.
To learn more about the Mulva Clinic for the Neurosciences, call 1-833-UT-CARES (1-833-882-2737) or visit here.