Tackling Alzheimer’s Disparities Among Hispanic Older Adults
UT Health Austin clinician-researchers work to understand and address the elevated risk of Alzheimer’s disease among Hispanic older adults
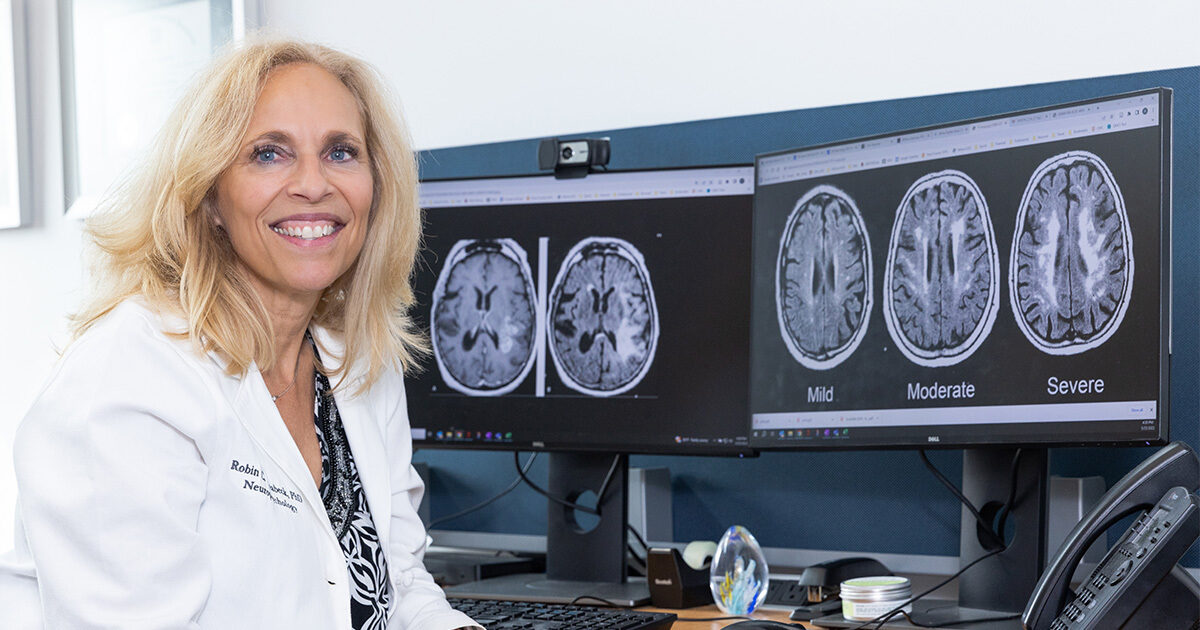
Reviewed by: Robin Hilsabeck, PhD, ABPP
Written by: Lauren Schneider
According to the Alzheimer’s Association, Hispanic older adults are at a disproportionate risk for Alzheimer’s disease in the United States, with some studies estimating that Hispanic older adults are 1.5 times more likely to develop the condition than White older adults.
Among the researchers seeking the root causes of this disparity is board-certified neuropsychologist Robin Hilsabeck, PhD, ABPP, who serves as the Director of UT Health Austin’s Comprehensive Memory Center within the Mulva Clinic for the Neurosciences. She oversees the clinic’s involvement in a multi-site initiative focused on Alzheimer’s outcomes within the Hispanic population alongside three other member institutions of the Texas Alzheimer’s Research and Care Consortium (TARCC), including The University of Texas Southwestern Medical Center, which is coordinating the project.
“The increased incidence of Alzheimer’s disease within the Hispanic population seems to be largely related to socioeconomic and environmental factors rather than genetics, meaning that these aspects are preventable,” says Dr. Hilsabeck. “If we can identify which factors drive condition onset, intervene early, and put protocols in place for risk management, we can decrease the prevalence of Alzheimer’s disease.”
Taking a Comprehensive View of Alzheimer’s Disease Risk
Over the next several years, Dr. Hilsabeck and her team will study how the onset of Alzheimer’s disease differs between individuals who identify as Hispanic and other older adults. Participants who have experienced any form of memory loss, regardless of whether they have been diagnosed with Alzheimer’s disease, will undergo a comprehensive annual exam that will both track disease progression and determine variables that may drive the condition.
Several strategies will be employed to measure disease progression, including a cognitive evaluation, a magnetic resonance imaging (MRI) scan to identify structural issues in regions of the brain known as the cortex and the hippocampus, and blood tests to measure expression of genes associated with Alzheimer’s disease as well as levels of both inflammatory compounds and the proteins amyloid-beta and phosphorylated-tau, which are believed to play a role in the condition. Participants can also opt for a spinal tap to analyze their cerebral-spinal fluid, allowing researchers to measure the presence of disease-associated compounds in the nervous system more accurately.
Medical issues linked to Alzheimer’s disease that affect certain populations at higher rates are also being assessed as potential risk factors. “While scientists are still working out the exact relationship between the conditions, metabolic syndrome–the combination of hyperlipidemia, hypertension, obesity, and high blood sugar– is associated with increased risk of Alzheimer’s disease,” notes Dr. Hilsabeck. “These conditions are more prevalent in African American and Hispanic communities for a number of cultural and environmental reasons, including decreased access to healthy food choices in historically Black and Hispanic neighborhoods.” Other factors that may contribute to elevated risk of Alzheimer’s disease include lack of access to enriching educational opportunities during youth and lifetime exposure to environmental toxins.
Adding the UT Health Austin Perspective
While the overall goal of evaluating Alzheimer’s disease risk among Hispanic older adults is shared by all four institutions involved in the project, Dr. Hilsabeck has a special interest in the role that chronic inflammation from environmental and medical stressors may play in accelerating neurodegenerative decline.
“Chronic immune system activation is thought to be related to the onset of Alzheimer’s disease,” explains Dr. Hilsabeck. “We predict that people of Hispanic and other minority backgrounds experience more chronic inflammation across their life due to adverse experiences, such as structural racism and discrimination, as well as from higher rates of medical comorbidities that cause inflammation.”
Another aspect of the initiative unique to Dr. Hilsabeck and her team is spearheaded by UT Health Austin neuropsychologist Jared F. Benge, PhD, who seeks to determine whether a person’s newfound difficulties using technology may be an early sign of cognitive impairment. The project is an extension of his broader interest in the role technology can play in the lives of older adults at risk for cognitive decline.
Led by clinical social worker Alyssa Aguirre, LCSW, UT Health Austin clinicians will also investigate how dementia caregiver burden differs between Hispanic and non-Hispanic caregivers. These findings could enhance the Comprehensive Memory Center’s ongoing efforts to support
those caring for loved ones with dementia.
UT Health Austin researchers are currently recruiting individuals ages 50 and older to take part in the study. Additional details are available in both English and Spanish. Those interested in enrolling can contact Bertha Ortiz at 1-512-495-5871 or tarcchispanic@austin.utexas.edu.
Moving Toward Culturally Informed Alzheimer’s Care
The results of this multi-site research initiative could have broad implications for Alzheimer’s disease prevention and treatment, including advancements in diagnostic testing methods. Currently, Alzheimer’s disease is believed to be under-diagnosed among Hispanic older adults, who are less likely to have health insurance, and those who do have access to treatment may not receive appropriate screening.
“Existing screening norms were first developed using data from non-Hispanic White patients,” shares Dr. Hilsabeck. “We need to ensure these norms are relevant to individuals of all different cultural backgrounds.”
Learn how the Comprehensive Memory Center is developing screening tools to identify cognitive impairment sooner.
<br>Understanding the factors that drive higher rates of Alzheimer’s disease in Hispanic older adults could impact care for people of all ethnicities. “Alzheimer’s disease is a complicated condition that is likely caused by more than one mechanism,” says Dr. Hilsabeck. “The ultimate goal is to develop a precision medicine approach to the disease. In the future, doctors will factor how a patient’s environment, genetics, and culture interact and use this information to tailor a treatment to their individual needs.”
For more information about the Comprehensive Memory Center or to schedule an appointment, call 1-833-UT-CARES (1-833-882-2737) or visit here.
To learn more about the Mulva Clinic for the Neurosciences, call 1-833-UT-CARES (1-833-882-2737) or visit here.