Managing Treatment-Resistant Depression With Transcranial Magnetic Stimulation
UT Health Austin psychiatrist explains the basis and benefits of the technique and describes what patients can expect from the procedure
Reviewed by: Nicholas Ortiz, MD
Written by: Lauren Schneider

Patients with major depressive disorder who have not responded to traditional treatments such as talk therapy or antidepressants should consider transcranial magnetic stimulation (TMS), says Nicholas Ortiz, MD, who serves as the Treatment Resistant Depression Director and Clinical Director of Neurostimulation at UT Health Austin.
How It Works
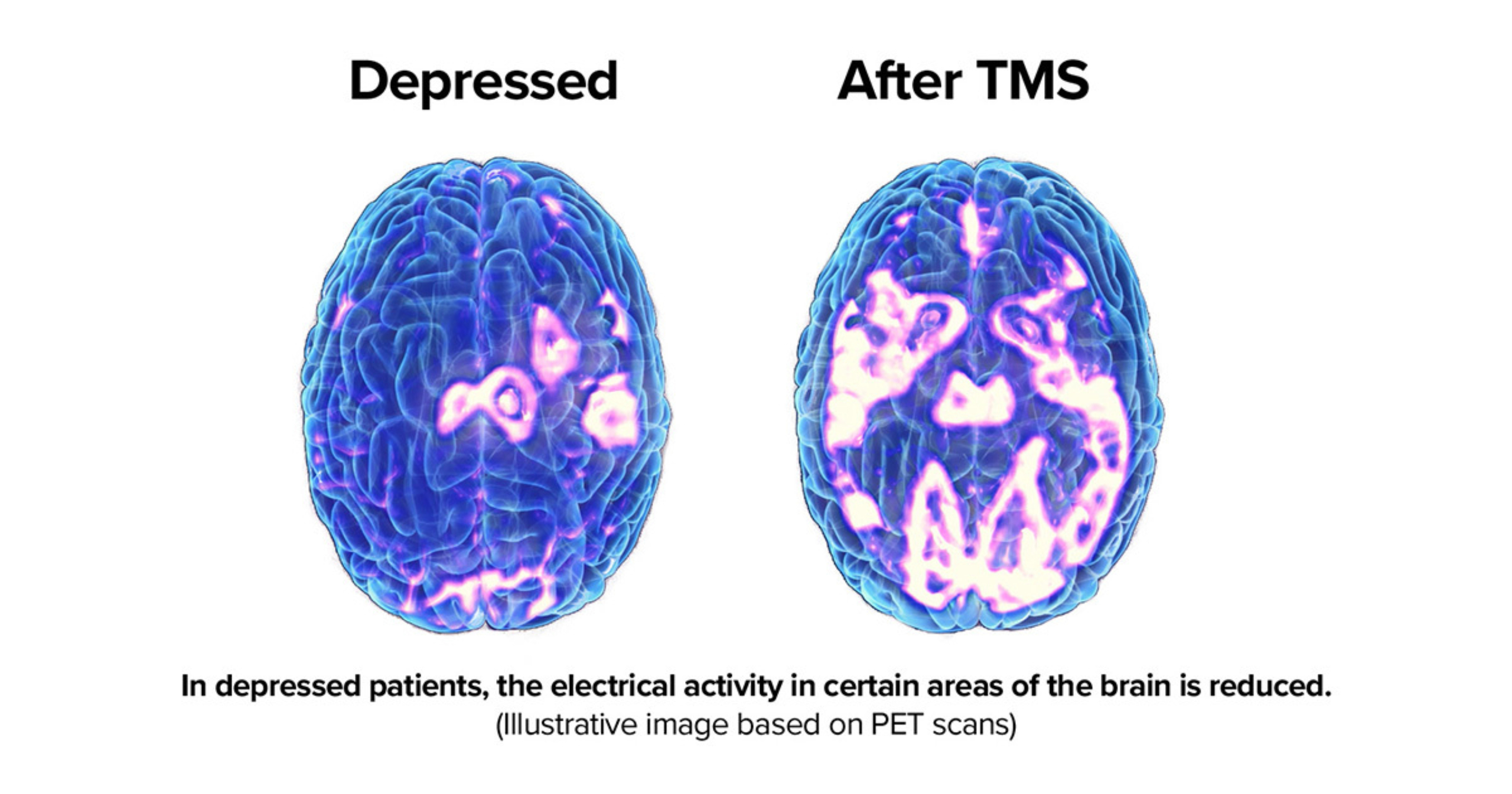
TMS is a noninvasive procedure that harnesses electromagnetic principles to activate neurons in a brain region of interest. During a TMS session, an electromagnetic coil is placed on the patient’s scalp. An electric current is sent through the coil, creating a magnetic field that in turn induces the electrical activity that triggers neuronal firing.
While this stimulation is only applied for a matter of minutes in a session, Dr. Ortiz says that regular TMS sessions can produce longer-term improvements in the activity of certain neuronal circuits.
“Repeated stimulation can change the way a network is functioning and allow that network to function in a healthier way, resulting in patients having fewer depressive symptoms.”
A Targeted Approach to Depression Treatment
According to Dr. Ortiz, “psychiatric medicines are effective, but plagued by side effects.” TMS may minimize these side effects for patients because the procedure only targets select areas of the brain. Pharmaceutical treatments, which circulate through a patient’s whole system, can exert unwanted effects on more tissues both within the brain and beyond.
Like most other clinics that use the technology to alleviate depressive symptoms, TMS treatment at UT Health Austin stimulates neurons in a region called the left dorsolateral prefrontal cortex (left dlPFC). Not only is this structure typically underactive in depression, with traditional approaches like pharmacotherapy and psychotherapy known to improve function in the area, but the dlPFC also sends signals to structures beyond the cortex that couldn’t otherwise be reached by TMS. Many of these sub-cortical regions, including the amygdala, insula, and anterior cingulate cortex, play important roles in emotional processing.
Accelerated and Accessible
In traditional TMS, each session typically lasts about half an hour. UT Health Austin utilizes a newer form of TMS called intermittent theta burst stimulation (iTBS) in which changes in the timing of pulse delivery shorten the treatment time to around five minutes per session. Dr. Ortiz cites a 2018 study that found iTBS is comparable to traditional TMS in terms of safety and efficacy. “That study really pushed the field to adopt iTBS.”
Shorter session times associated with iTBS make the procedure more accessible in two ways: not only does a smaller time commitment make TMS feasible for more patients, but doctors are able to treat more patients in a given period.
What Patients Can Expect
Before beginning TMS treatment at UT Health Austin, patients meet with a care team for a consultation, during which the care team will assess whether the patient is a good candidate for the procedure. Patients start out with 5 weekly sessions for the first 4-6 weeks of treatment. The number of treatments per week will then taper off, decreasing by one session per week.
Patients seeking TMS at UT Health Austin are not required to have a referral from another doctor, but it is recommended that they have a primary care provider or a psychiatrist.
Dr. Ortiz cautions against patients abandoning other depression management strategies while during this process. “I wouldn’t recommend TMS in a vacuum.”
“Talk therapy alongside TMS is a very important aspect,” he says, adding that patients for whom antidepressants have been partially helpful should also continue their pharmacotherapy regimen in a tolerable manner. “I also ask our patients to have a regular sleep schedule, regular exercise schedule, and we talk about diet choices.”
The most common side effect associated with TMS is a mild headache, which Dr. Ortiz attributes to the mild discomfort patients experience when exposed to the magnetic field. “If that goes on for five minutes, some folks feel a little bit of focal head pain.”
Early in the development of TMS, practitioners feared that seizures may be a side effect of the treatment. “If stimulation parameters are done in an excessive manner, there is a theoretical risk of seizure that is documented to be about 1 in 50,000 treatments,” says Dr. Ortiz, adding that this risk number has declined as more treatments continue to be performed. He points out that patients with epilepsy can safely undergo TMS, further underscoring the safety of the procedure.
Long-Term Outcomes
The functional changes evoked by TMS are long-lasting, but they are not permanent. According to Dr. Ortiz, the effects of the treatment last for a variable amount of time, lasting longer in younger patients and those who undergo more treatments.
“The literature suggests that at about four to six months, the majority of patients are still able to realize improvement in their symptoms,” he says. “We’re hoping for more durable options and there’s evolving research about maintenance TMS.” On a maintenance treatment course, patients would continue to undergo TMS sessions on a regular basis to prevent symptom relapse.
However, as the nature of TMS treatment evolves, Dr. Ortiz is optimistic about the future of the procedure. “TMS is still in its infancy and the research around its effectiveness is growing so rapidly. I anticipate that it’s going to be a great resource for patients”.
For more information about TMS, or to schedule an appointment visit here.