HPV Is Still Flying Under the Radar
It’s not just a woman problem, it’s an every person problem
Reviewed by: Lauren Thaxton, MD
Written by: Lauryn Feil

You’ve likely heard of HPV, or human papillomavirus (if you haven’t, don’t worry, you came to the right spot); you’ve chosen to (or not to) get the vaccine; you know it’s sexually transmitted; and you’ve been told to use protection, get regular STD tests, or to visit your doctor if you notice something aloof after sexual intercourse. Easy-peasy, you get it, right?
Not so fast, let’s take a step back. HPV isn’t that simple, and many people don’t know that much about it. For starters, if you’re sexually active, you likely have or likely will be exposed to HPV at some point in your lifetime. You’re probably thinking, “Pssht, no way, not me.” But seriously, 4 out of every 5 people (a whopping 80%) will contract the virus, and according to the Centers for Disease Control and Prevention (CDC), 79 million Americans are currently infected with HPV. Has your jaw hit the floor yet? Don’t be too alarmed, just keep reading!
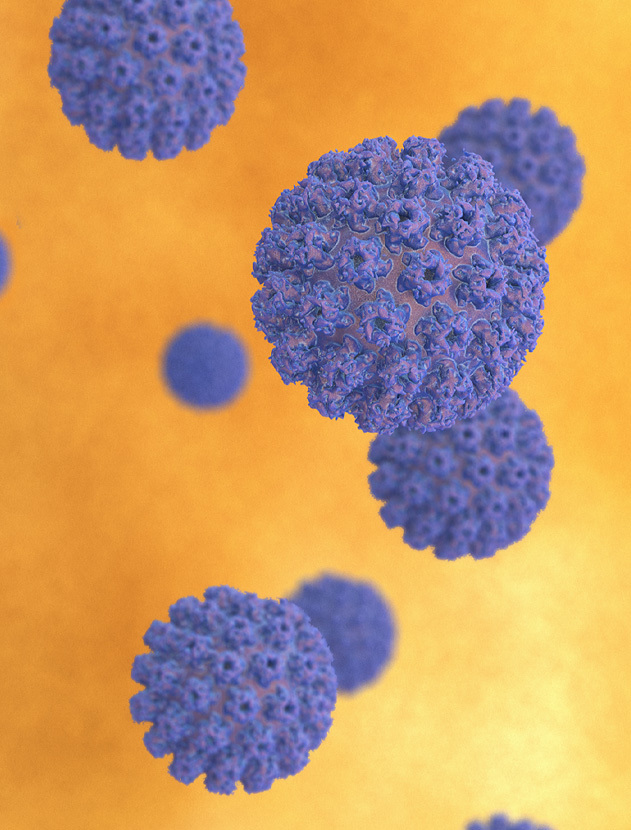
Let’s start with the basics, what exactly is HPV?
HPV is the most common sexually transmitted infection. There are about 200 types of HPV – 40 of which can be spread through direct sexual contact (which is the focus of this article). Some strains cause oral and genital warts, other types cause cancer or precancerous lesions, and some strains just go away entirely on their own. 99% of cervical cancers are caused by HPV, and HPV is also linked to certain types of oral cancers and other cancers of the genitals as well as head and neck cancers. The virus infects the skin and moist membranes such as the lining of the mouth and throat, the cervix, vagina, vulva, anus, and penis.
How does HPV spread?
You can get infected with HPV by having any kind of sexual contact – vaginal, anal, and oral – with an infected partner, even if they are not showing signs or symptoms (like genital warts). The virus is spread mainly through skin-to-skin contact, not through bodily fluids or blood. This means genital-to-genital contact without penetration and even kissing (although rare) can spread HPV. Using protection (like condoms) during intercourse can help reduce risk of infection, but it is not guaranteed. The upside: You can’t get HPV in a hot tub or pool, from a toilet seat, or by sharing food.
Who is at risk for getting HPV?
The short answer: Anyone having sex. If you are engaging in sexual intercourse, you are at risk of exposure. Clinicians will agree that the more sexual partners you or your partner have, the higher your risk of contracting HPV. The CDC also notes that even if you’ve only had one sexual partner, you can still contract the virus as symptoms can sometimes develop years after having sex with someone infected.

What are the symptoms of HPV?
Aside from the strains that cause genital warts, other low- and high-risk HPV strains do not cause any symptoms at all. Warts typically appear in the genital area or around the mouth within a few months after you’ve been exposed. They appear as small fleshy, painless bumps that are one to two millimeters in size and can be treated. In women, if you have developed an HPV-related precancerous or cancerous lesion on your cervix, it can sometimes cause irregular bleeding and bleeding after sex. Unfortunately, there is no way to screen for HPV in men and the only reliable way to test for HPV in women is through regular Pap smears, which involve collecting the cells from your cervix and testing them for any abnormal changes. An irregular Pap test can be the first red flag that you’ve contracted HPV.
How is HPV treated?
For most people, both low- and high-risk HPV infections go away on their own in one to two years and the infection does not require any special treatment, meaning your immune system takes care of everything. If you receive an irregular Pap test, your physician may want to perform a colposcopy where they use a magnifying device called a colposcope to get a better look at the cell abnormalities on your cervix. They may also take a small sample of the abnormal tissue to biopsy. Patients are typically advised to return for a follow-up Pap test or other procedures based on their doctor’s recommendations.
Genital warts can also go away on their own, or they can be removed by freezing, burning, or lasering, similar to how you would treat warts on your hands or feet. There are topical creams that can reduce the size of warts as well.
Is there any way to prevent HPV?
Using condoms during sex can reduce odds of infection due to less direct skin-to-skin contact, but they only offer partial protection, so infection can still occur. The most effective preventative method against HPV is the vaccine known as Gardasil 9.

This vaccine protects you against the following HPV strains that lead to cancer or genital warts:
- HPV types 16 and 18 — the 2 types that cause 80% of cervical cancer cases
- HPV types 6 and 11, which cause 90% of genital warts cases
- Another 5 types of HPV (types 31, 33, 45, 52, and 58) that can lead to cancer of the cervix, anus, vulva/vagina, penis, or throat
The HPV vaccine is given in a series of shots:
- For people ages 15-45, the HPV vaccine is 3 separate shots given over the course of 6 months; once the first shot is administered, the second shot is given 2 months after the first, and the third shot is given 4 months after the second
- For people ages 9-14, patients only need to get 2 shots; after the first shot is administered, the second shot is given 6 months later
All people ages 9-45 can get vaccinated to protect themselves from cancer causing strains. (Note: This is latest recommendation from the CDC, although many insurance companies only cover the vaccine up to age 26.) The vaccine is extremely safe, and children are recommended to get the vaccine at age 11 or 12, so they’re fully protected, ideally, before they become sexually active.
If you already have HPV, the vaccine will not help treat your current infection, but it can help protect you from other strains of HPV. The vaccine does not protect against ALL strains of HPV, only the higher-risk ones, so you may still contract the virus, but it will likely clear on its own without further treatment. Talk to your healthcare provider about what treatment may be best for you.
Don’t panic, get informed.
An HPV diagnosis does not reflect negatively on you, or anyone for that matter. As mentioned before, 80% of people contract HPV at least once in their lifetime, the virus is extremely common, and it typically goes away on its own. So really, there’s nothing to be ashamed of.
You can, however, get informed, help inform others, and get vaccinated. 13,000 women in the United States are diagnosed with cervical cancer each year and thousands of other people are diagnosed with HPV-related cancers. We, meaning everyone – men, women, and people of all genders – can help reduce those number and save lives. The Gardasil 9 vaccine is the only vaccine against cancer, so why not play it safe?
For more information or to make an appointment with UT Health Austin, visit here or call 1-833-UT-CARES (1-833-882-2737).