Bridging Gaps in Cervical Care
New technology aims to bring more accessible cervical cancer screening to underserved communities throughout Central Texas
Reviewed by: Shreya Ahuja, Rabab Isa, and M. Yvette Williams-Brown, MD, MMS, FACOG
Written by: Lauren Schneider
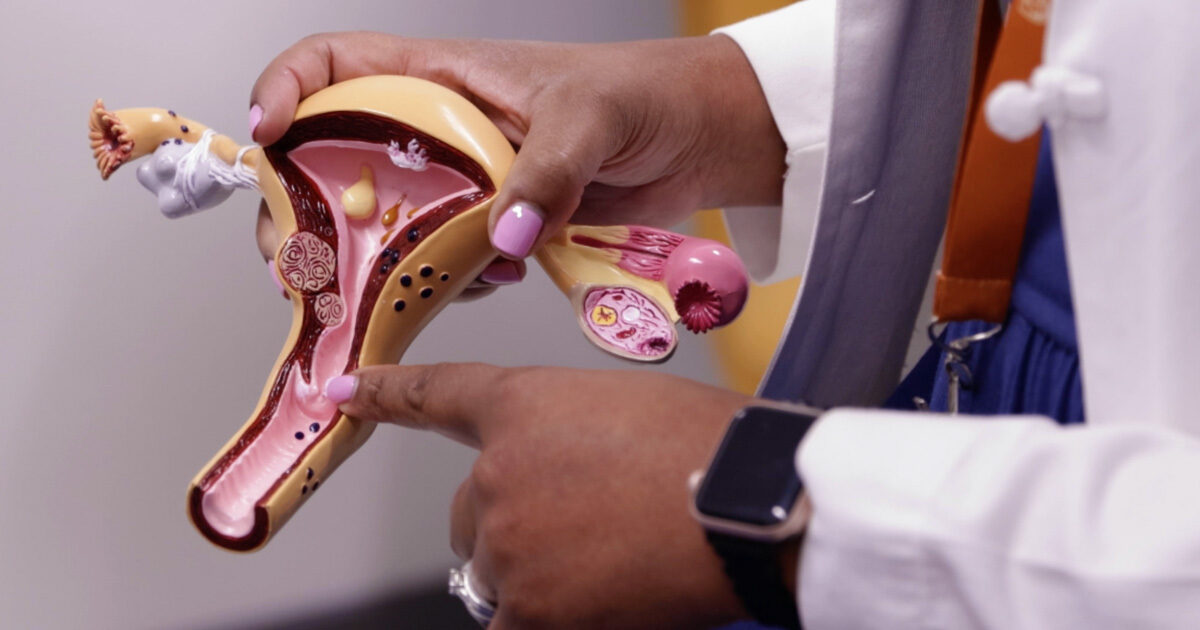
A new project will evaluate the role of portable devices in cervical cancer screening and prevention in communities without the resources to provide a standard colposcopy exam in a traditional clinical setting. Funded by a Health Equity Pilot Project Award from the Office of Research and Office of Health Equity at the Dell Medical School, the study will gather feedback about the portable colposcope’s usability and benefits from providers treating underserved populations in mobile clinics across Central Texas.
“Standard colposcopy is a specialized diagnostic procedure that follows an abnormal cervical cancer screening test. This procedure typically requires the use of very expensive equipment, so only clinics with adequate expertise, funding, and volume will usually purchase a traditional colposcope,” explains M. Yvette Williams-Brown, MD, a fellowship-trained gynecologic oncologist in Women’s Health, a clinical partnership between Ascension Seton and UT Health Austin. “The portable version of the colposcope is useful in settings where there is a high prevalence of cervical cancer or pre-cancer but, due to a lack of resources, people may not have easy access to a clinic where they can have a colposcopy performed.”
Read more from Dr. Williams-Brown about cervical cancer screening.
The study was initiated by Shreya Ahuja and Rabab Isa, two rising fourth-year students at the Dell Medical School, and will build on prior knowledge about the pocket colposcope by studying its use in underserved communities in the United States. While the device is approved by the Food and Drug Administration (FDA) for cervical cancer screenings, previous research has largely focused on the global setting.
“Research involving the pocket colposcope has mostly taken place in other countries,” notes Rabab. “Our goal is to understand the usability of the device from a provider’s perspective in a low-resource setting in the United States to help combat health disparities closer to home.”
From a Classroom to the Community
Shreya became aware of the pocket colposcope during her time as an undergraduate student at Duke University, where the device was first developed at the university’s Center for Global Women’s Health Technologies (GWHT). When she took a position at Kaiser Permanente after graduation, she became acquainted with the founder of GWHT, affording her insight into the technology’s continued development.
In her second year at the Dell Medical School, during her obstetrics and gynecology (ob-gyn) rotation, Shreya wrote a report about the pocket colposcope as part of her program’s health equity assignment in which students are prompted to identify a gap in healthcare outcomes and explore possible solutions. “After the assignment, I started asking myself how I could turn that report into a tangible project to benefit the community,” explains Shreya.
Shreya’s first step in developing this project was to enlist fellow second-year student Rabab because of her interest in ob-gyn as a specialty. “As an aspiring radiologist, my interest lies in using novel imaging techniques to improve access to care for vulnerable populations, whereas Rabab’s focus is the ob-gyn perspective,” shares Shreya.
Shreya and Rabab reached out to Dr. Williams-Brown, who had previously shared her work on promoting health equity in gynecologic oncology to the students in the ob-gyn rotation as part of an educational session.
“We first approached Dr. Williams-Brown to see if a project with the pocket colposcope was even feasible in Texas, and since then she’s become the faculty advisor and a really great mentor for both of us,” says Rabab.
As a physician-educator, Dr. Williams-Brown serves as an associate professor in both the Dell Medical School Department of Women’s Health and the Dell Medical School Department of Oncology, where she provides education and training for the next generation of gynecologic surgeons. She also provides subspecialty training in minimally invasive gynecologic surgery as the Program Director of the Minimally Invasive Gynecologic Surgery Fellowship.
“While we may have understood the technology and we brought forth a research project idea, we didn’t fully understand the local healthcare landscape,” adds Shreya. “Dr. Williams-Brown offered that broader context because she’s done a lot of work in this community.”
Reducing Barriers to Cervical Cancer Screening
Through working with Dr. Williams-Brown, the students have gained greater appreciation for the obstacles many Central Texans face in accessing cervical care. “Cervical cancer is one of the most preventable cancers in the United States, and the fact that it still has such a high incidence and prevalence, especially in Texas, speaks to disparities in preventive care,” says Rabab. “Patients who are traditionally underserved, such as those who have come from a lower socioeconomic or health literacy background, are prone to falling through the cracks.”
While socioeconomic factors drive countless health disparities, cervical cancer screening presents a unique challenge to underserved patients, because it is a multi-step undertaking. “Barriers that prevent a patient from receiving care can affect each stage of the screening process. If a patient’s pap smear is positive, then they need to come back multiple times for further testing and be available for follow-up reports from the clinic. This can prove difficult when that patient lacks reliable transportation or internet to access a clinic’s patient portal,” notes Shreya. “We hope that the portable colposcope facilitates the screening process by making at least one of these steps more available to patients.”
The team expects to collect data related to the pocket colposcope throughout the summer and draft a manuscript documenting their efforts by August 2023. “Through this project, we aim to demonstrate whether the use of mobile colposcopy can help providers meet patients where they are,” says Dr. Williams-Brown. “By making screening more accessible, we can make cervical health more equitable.”
For more information about services available through Women’s Health, visit here.