Uveitis and Ocular Inflammatory Disease
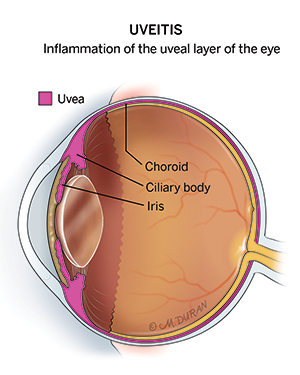
Uveitis is a term used to describe a group of inflammatory diseases that damage the middle layer of tissue in the eye wall, or uvea. The condition results in approximately 43,000 new cases in the United States each year. Uveitis specialists who treat uveitis also frequently manage other types of ocular inflammatory disease, which can lead to permanent vision damage. Early diagnosis and treatment by a uveitis specialist can help prevent complications and preserve your vision.
Types of Uveitis and Ocular Inflammatory Disease
The types of uveitis and other ocular inflammatory diseases are classified by which part of the eye is affected. For instance, scleritis describes inflammation of the wall of the eye, myositis describes inflammation of the muscles around the eye, and chorioretinitis describes inflammation of the back of the eye.
Examples of uveitis:
- Anterior uveitis:
- Uveitis associated with HLA-B27
- Uveitis associated with juvenile idiopathic arthritis (JIA)
- Fuchs heterochromic iridocyclitis
- Tubulointerstitial nephritis and uveitis syndrome
- Intermediate uveitis:
- Uveitis associated with multiple sclerosis (MS)
- Uveitis associated with Lyme disease
- Pars Planitis
- Posterior uveitis:
- Acute posterior multifocal placoid pigment epitheliopathy (APMPPE)
- Acute zonal occult outer retinopathy (AZOOR)
- Multiple evanescent white dot syndrome (MEWDS)
- Punctate inner choroidopathy (PIC)
- Panuveitis:
- Behçet’s disease
- Birdshot chorioretinopathy
- Multifocal choroiditis
- Toxoplasmosis chorioretinitis
- Vogt-Koyanagi-Harada disease (VKH disease)
Examples of ocular inflammatory diseases:
- Choroiditis
- Episcleritis
- Sarcoidosis
- Scleritis (often associated with underlying systemic diseases, such as rheumatoid arthritis and granulomatosis with polyangiitis)
- Ocular cicatricial pemphigoid (also known as mucous membrane pemphigoid)
- Orbital inflammatory syndrome:
- Orbital myositis
- Orbital pseudotumor
Symptoms of Uveitis and Ocular Inflammatory Disease
The signs and symptoms of uveitis and other ocular inflammatory diseases depends on the types of inflammation and can last for a short (acute) or long (chronic) time. The severest forms of ocular inflammation may reoccur several times over. Symptoms often come on suddenly and get worse quickly.
Early symptoms of uveitis and ocular inflammatory disease may include:
- A small pupil
- Changes in the color of the iris, the colored part of the eye around the pupil
- Decreased or blurred vision
- Eye pain
- Floaters (seeing specks or shadows) in the field of vision
- Photophobia, or sensitivity to light
- Red eye, redness around the eye, or bloodshot eyes
- Swelling and irritation
Late symptoms of uveitis and ocular inflammatory disease may include:
- Vision loss
Risk Factors for Uveitis and Ocular Inflammatory Disease
Uveitis and ocular inflammatory diseases often occur without an identifiable cause, but some people are more likely to develop the condition. However,
Risk factors for uveitis and ocular inflammatory disease may include:
- Family history: A family history of inflammatory conditions can increase your risk of uveitis or other ocular inflammatory disease.
- Health history: In some cases, ocular inflammatory conditions can be traced back to an eye injury, an infection (e.g., herpes, Lyme disease, shingles, syphilis, tuberculosis, etc.), or an autoimmune disease (e.g., inflammatory bowel disease, lupus, multiple sclerosis, rheumatoid arthritis, etc.).
- Personal history: Tobacco use is associated with uveitis and ocular inflammatory disease.
Treating Uveitis and Ocular Inflammatory Disease at UT Health Austin
Treatment is dependent on the underlying cause of the ocular inflammation, the severity of the disease, and which part of the eye is affected in addition to the patient’s overall health. Your first visit often takes 2-4 hours depending on the complexity of your case and any in-clinic testing that may be required. Your uveitis specialist is well-versed in the most current, evidence-based treatment recommendations, which may include medications (by mouth or injection) or surgery.
Care Team Approach
At UT Health Austin, we take a multidisciplinary approach to your care. This means you will benefit from the expertise of multiple specialists across a variety of disciplines. Your care team will include fellowship-trained ophthalmologists, ophthalmic technicians, physician assistants, nurse practitioners, social workers, and more who work together to help you get back to the things in your life that matter most to you. We also collaborate with our colleagues at the Dell Medical School and The University of Texas at Austin to utilize the latest research, diagnostic, and treatment techniques, allowing us to identify new therapies to improve treatment outcomes. We are committed to communicating and coordinating your care with your other healthcare providers to ensure that we are providing you with comprehensive, whole-person care.
Learn More About Your Care Team

Mitchel and Shannon Wong Eye Institute
Health Transformation Building, 1st Floor
1601 Trinity Street, Bldg. A, Austin, Texas 78712
1-833-UT-CARES (1-833-882-2737)
Get Directions